Yakkaphan, P., Elias, LA., Ravindranath, P. et al. Is painful temporomandibular disorder a real headache for many patients?. Br Dent J 236, 475–482 (2024).
Introduction
Temporomandibular disorders (TMDs) are a group of musculoskeletal conditions causing pain or functional limitations in the jaw muscles, temporomandibular joints (TMJ), and related structures in the orofacial region. Migraine is a subtype of primary headache condition characterised by headache attacks associated with autonomic disturbances, such as nausea, and increased sensitivity to external stimuli. Although they are two completely different disorders, there is much overlap which can lead to misdiagnosis or underdiagnosis of one or other condition. Furthermore, studies have suggested a bidirectional association between migraine and TMD and this review aims to explore this relationship.
Anatomical relationship between TMD and migraine
Anatomically, migraine pain commonly occurs in the ophthalmic branch of the trigeminal nerve (V1) which can occasionally radiate to the V2 and V3 branches. During the onset of migraine, many patients experience spontaneous pain in the teeth, cheek, masticatory muscles and periauricular region. Such presentations of migraine can be misdiagnosed as TMD, odontogenic pain or sinusitis. As a result, this can potentially lead to inappropriate treatment such as extractions. Furthermore, the distribution of migraine pain was found to be similar to TMD, radiating widely in the cranial and orofacial regions.
Pathophysiological perspectives
One of the possible links between migraine and TMD is peripheral and central sensitisation, where normal or sub-threshold stimulators from TMJ and associated structures may become migraine-inducing factors or vice versa. For example, myofascial trigger points (MTP) are sensitive areas in the muscles which can elicit pain. These areas, located in the muscles of mastication, are common in both TMD and migraine.
TMD and migraine may also trigger each other due to cross-excitation of trigeminal fibres. Although the dura mater is innervated mainly by the V1 branch, it is also supplied by the branches V2 and V3. This can explain why migraine pain may occur in the V2 and V3 regions.
Neuromusculoskeletal dysfunction of the cervical spine has been found to contribute to both TMD and migraine via the trigeminocervical complex (TCC). The convergence of the nociceptive pathways of the upper cervical spine and the trigeminal system can refer pain signals from the neck to the trigeminal sensory receptive fields in the face and head.
On a molecular level, the release of proinflammatory molecules could play a role in the sensitisation and association between TMD and migraine. In particular, the level of CGRP is significantly higher in TMD patients and there is a positive correlation between the magnitude of CGRP levels and pain intensity. This can then lead to the excitation of peripheral and meningeal afferents and the development of migraine.
Differentiation of TMD and migraine
The aim of the clinical assessment is to determine the underlying cause of TMD pain, distinguishing between cases in which TMD is comorbid with migraine and cases in which migraine pain mimics TMD. Migraine symptoms can be assessed by inquiring about headache-related disability, nausea, and sensitivity to light in the past three months
Regarding the clinical examination for diagnosing TMD, reproducible pain on TMJ and masticatory muscle palpation play a crucial role in diagnosing TMD, it is important to be cautious of myofascial pain among individuals with migraines. As a result, this review suggests to exclude migraine in patients with positive TMD symptoms.
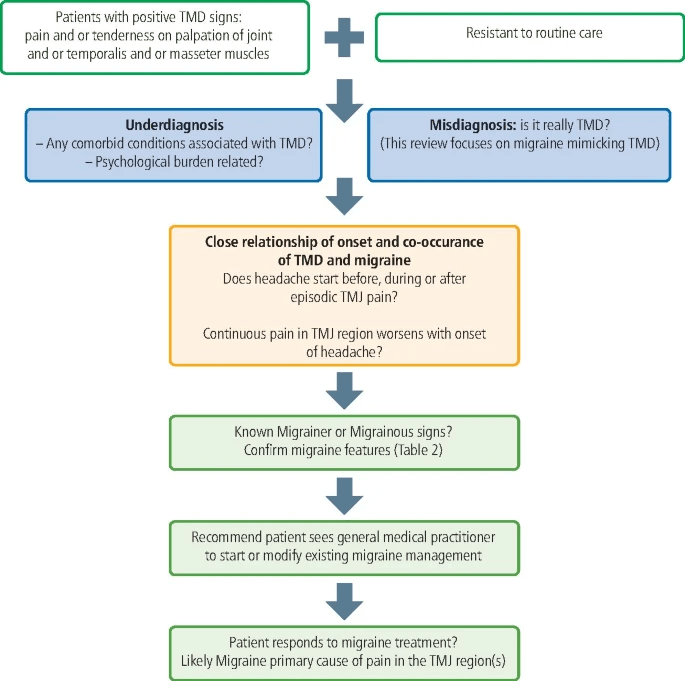
Fig 1: Diagnostic scheme for excluding migraine in patients with TMD symptoms.
Headache or migraine attributed to TMD
Although migraine can behave similarly to TMD pain, TMD can also induce headaches, and this is known as headache attributed to TMD (HATMD). The confirmation of familiar headache when jaw movement or muscle palpation during clinical examination is key for identifying HATMD.
Individuals with migraine pain who are found to have TMD pain as the source of migraine should be diagnosed as having migraine attributed to TMD. Therefore, solo TMD treatment, not additional headache treatment, may be sufficient to improve the headache. Research has shown a significant correlation between a reduction in TMD symptoms and a decrease in the frequency and intensity of headaches. Conversely, if the TMD symptoms originate from migraine, as described above, a single TMD treatment will not benefit these patients. Therefore, the response to treatment may be a hint to helping the clinician determine the true cause of the pain.
Conclusion
TMD and migraine are prevalent and highly inter-related. Distinguishing TMD and migraine can be challenging, especially when both disorders co-exist in a single individual. Therefore, it is essential to exclude migraine and other primary headaches that can potentially cause or exacerbate TMD symptoms, thus ensuring that the patient receives appropriate treatment. This review also shows a need for further studies to prove the link between TMD and migraine headaches and provide more effective treatment.
Research Summary Written By: Hewitt Yau, Newcastle University – BDS5
