Finn K, Moore D, Dailey Y, Thompson W. The use of oral benzodiazepines for the management of dental anxiety: a web-based survey of UK dentists. Br Dent J. 2023 May 24:1–5. doi: 10.1038/s41415-023-5850-5.
Background
Dental anxiety is a common issue that dental professionals encounter regularly with patients, with more severe reports in 12% of the adult population. It is a key aspect of patient care as those who experience anxiety around dental treatment often have poorer attendance and oral hygiene as well as an increased risk of untreated disease. Therefore, non-pharmaceutical and pharmaceutical methods are the management options of choice, from cognitive behavioural therapy to conscious sedation, however there is a significant discussion in relation to the use of oral benzodiazepines (OBZs).
Methods
This article utilises an online questionnaire of 235 eligible dentists where participants were recruited via a private Facebook group in 2021, to which the majority, at 91%, were general dental practitioners and overall, mostly were women, at 59%.
Results
Despite having half of the participants previously prescribing OBZs, only 18% of those were assured that they had sufficient knowledge to do so. Compared to dentists who recently qualified, those who obtained their qualification over thirty years ago were twice as likely to have prescribed these drugs. Diazepam was discovered to be the favoured OBZ prescribed despite the BNF recommendation for the use of Temazepam; this is preferred due to its shorter half-life and minimal chance of interactions in comparison, limiting the side effects that follow. OBZ prescription timings by the respondents were slightly varied, with most suggesting prescriptions for the night before and 1-2 hours before the procedure. Surprisingly, lack of confidence in their knowledge of prescribing these drugs included 1 in 4 of the responses; 1 in 3 responses involved the use of a general medical practitioner to alternatively prescribe the drug although this presents multiple issues as patient’s consent can be compromised, confusion with the medical history as dentists may not have access to full medical records, and therefore presents risks to patient safety.
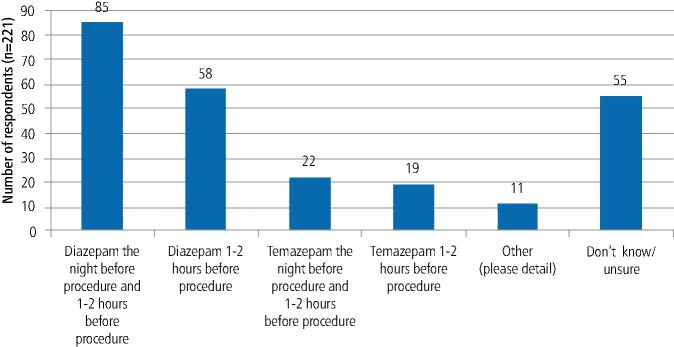
Fig. 1 Preferred OBZ prescribing regimen for a fit and well anxious adult to facilitate the surgical removal of a tooth (participants could select more than one option, therefore the total number of responses is greater than the number of respondents) (Finn et al., 2023).
There are several benefits to OBZs in anxiety management, such as increasing patient cooperation, since they feel more comfortable, and reducing the waiting lists for sedation; a significant disadvantage is the abuse and dependence on OBZs which discouraged many dentists from prescribing.
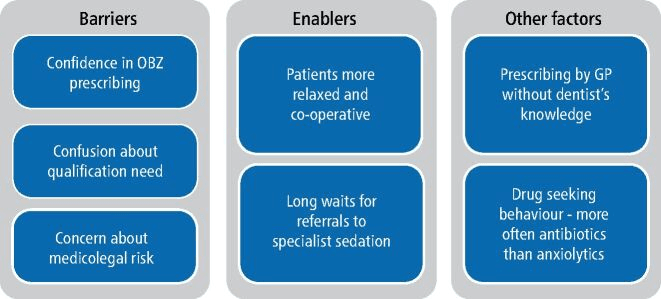
Fig. 2 Summary of barriers, enablers and other complicating factors (Finn et al., 2023).
Conclusion
The study suggests moving forward, that further education and training is required in the prescription of OBZs, including clarity within the guidelines available and relevant qualifications required. It is important for dentists to understand the role of the GP in these prescriptions and in future, having access to patient’s complete medical history can both ensure patient safety is taken into consideration when dentists are also prescribing. Overall, developing more supportive pathways for dental anxious patients for all dental professionals requires further, clearer guidance.
Research Summary Written By: Jessica Evans, Cardiff University – BDS4
